SPINE SURGERY-PROBLEMS AND INNOVATIONS. ARTICULATED LUMBAR
CAGE.
Author: Munir Elias.
M.D, Ph.D. in neurosurgery and human neurophysiology.
Abstract
Background:
Spine surgery is the most common problem facing the neurosurgeon and
certain group of orthopedics. It consist over 90% of the activity of
the general neurosurgeon in private sector. The most important and
most common operations are the lumbar disc surgery and among the
most common complications are recurrent disc and discitis. Recurrent
lumbar disc, which needs reoperation is around 3-18%. Recurrent
cervical disc surgery is almost near zero. All the available today
methods to resolve this problem are not acceptable, because
transpedicular fixation of the segment have its complications and
negative drawbacks by itself. A trail to perform bilateral cleaning
of the disc space increase the rate of recurrence. Bilateral
cleaning with insertion of 2 TLIF cages from each side also
dynamically have its hazards. The below mentioned data and
suggestions are the answer to provide the best solution to make the
lumbar disc recurrence around zero as in the cervical area without
causing further bony destruction to the surrounding anatomical
structures.
Methods:
Since in the industry, there is no such device, the author start to
acquire engineering knowledge about the industry of spinal
instrumentations and the biomechanics of the lumbar spine and using
software such as SolidWorks, Autodesk Inventor and ORS Visual to
resolve the problem. Starting from August 2016 up to now, several
versions of cage construction were improvised and improved over more
than 40 versions. The cage must be MRI compatible without artifacts,
slim, not migrating and have several fixating points within the disc
space and providing the normal lordotic anatomy of the area.
Results:
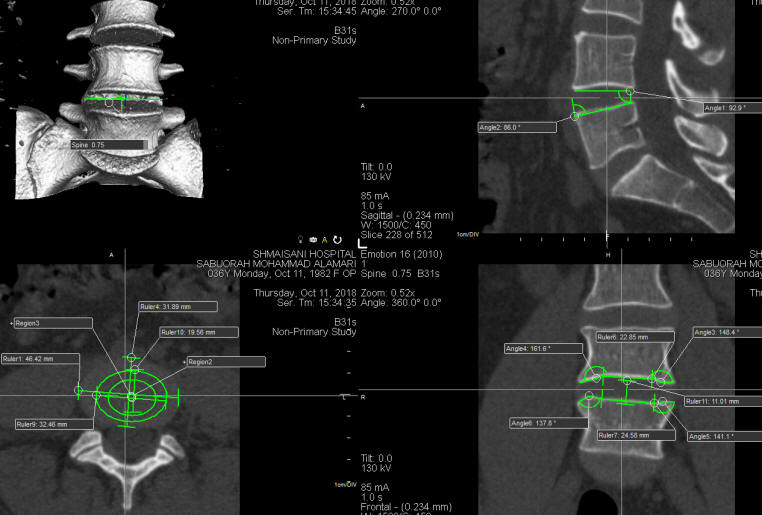
More than 300 cases of the lumbar area were sent for CT-scan L2-S1
with thin continuous cuts and using ORS Visual software and area was
studied with accuracy. Each segment of the the lumbar area have its
unique characteristic, but L2-3, L3-4 and L4-5 share some
similarity. L5-S1 have a little different characteristics. The
lordosis in these segments was ranging from 6 to 14 degrees. The
inner shape of the disc space had some depth around the elevated
center in the inferior wall of the disc space. This trough is around
30 mm in diameter from the outer circumference for most of them with
tiny deviation.
Conclusions:
Lumbar articulated cage with double self-locking mechanism is the
most suitable solution to minimize the postoperative lumbar disc
surgery recurrence rate without the need to violate further
anatomical structures.
Keywords: Articulated lumbar cage, recurrent lumbar disc, neurosurgery, spine
surgery
INTRODUCTION
Neurosurgery and spine surgery have a lot of challenges. Recurrent
prolapsed lumbar disc requiring surgery, is among the most frequent
problems annoying the life of the patient and the neurosurgeon, for
what many articles were written and among them by myself.
1
A group of 18 patients were operated by me with insertion of
Medtronic Satellite sphere ended with complications, for what it was
abandoned. In retrospective analysis of this group, the sphere cause
avascular necrosis of the upper and lower vertebrae. It then
creating tunneling inside the disc space, permitting the sphere to
migrate inside the disc space with in these tunnels and the patient
coming with different scoliotic posture every postoperative visit.
Insertion of TLIF PLIF ALIF must be accompanied with transpedicular
fixation of the adjacent involved segments. Some authors suggested
insertion of 2 TLIF from each side after bilateral cleaning of the
disc space.2 The suggested trabicular cage has many
disadvantages, among them, no respect to the lordotic nature of the
area and no connection between the 2 devices and and massive
MRI artifacts. Pedicular
screw fixation for simple prolapsed lumbar disc is relatively
unacceptable to prevent the recurrence and the complications with
some authors reach up to 54%. 3 The improvement of
the pedicular screws will not be acceptable in simple lumbar disc
prolapse, even if the complications reach 0%, because this technique
will violate further anatomical structures.
Schmorl's nodules have common place in the vertebral
spine and some authors claim it could cause back pain, for what some
surgeons perform transpedicular fixation of the involved segment.4
With the 40 years experience of the author, this kind of herniation
mostly is not the cause of pain by itself, but the disturbance of
biodynamics of the segment can be the cause. I never paid attention
to this kind of "pathology", because it is a frequent finding and
most of the patients coming with other causes of their essential
pathology. This fact was mentioned, because most of the Schmorl's
nodules are central in location and the cage will avoid their
location.
For pain management of the
radicular pain, the author have now wide experience with application
of bipolar mode radiofrequency to the involved roots during
discectomy and it yield a good result.5
In high index of suspicion for
discitis or presence of infection in other parts of the body, the
patient usually is treated for his infection before surgery. Despite
this fact infection will resume even several weeks after surgery in
some cases, necessitating long term treatment with antibiotics. The
insertion of the cage with the bone graft and the area aided with
Vancomycin powder could decrease this possibility. The escalation of
osteomyelitis of the adjacent vertebrae could enforce the surgeon to
remove the construct, for what the device was constructed to be
easily removed.
MATERIALS AND METHODS
Anatomical background:
The disc is a fibrocartilage that lies between bony
vertebral bodies, conferring flexibility, load transfer, and energy
dissipation to the spine. It is comprised of the central gelatinous
nucleus pulposus (NP) surrounded circumferentially by the annulus
fibrosus (AF). The hyaline cartilage endplate forms an interface
between the disc and adjacent vertebral bodies. The NP is
structurally and mechanically isotropic and contains a network of
type II collagen interspersed with proteoglycans, resulting in a
high water content within the tissue. The osmotic swelling that
results is a defining feature of NP mechanics. Each lamella of the
multi-lamellar AF consists of highly aligned collagen fibers whose
orientation alternates above and below the transverse axis of the
spine by approximately 30° in adjacent lamellae. While the AF can be
approximated as an angle-ply laminate ring, its true architecture is
more complex: lamellae are circumferentially discontinuous and
traversed by fibrous elements that run radially outward.6
The authors in their article mentioned the importance of the annulus
fibrosis and nucleus fibrosis and described in detail the
biomechanics and bioengineering and they mentioned the following:
Fusion is the surgical standard for the treatment of axial low back
pain. This treatment is highly invasive and is intended to stop pain
by eliminating motion across the joint space. Despite the frequency
of its practice, fusion often fails to alleviate pain and may
accelerate degenerative changes in adjacent discs. Total disc
arthroplasty is a recently approved surgical option that aims to
maintain segmental motion; however, its long term efficacy has not
been established and mechanical wear may challenge its the long-term
success.
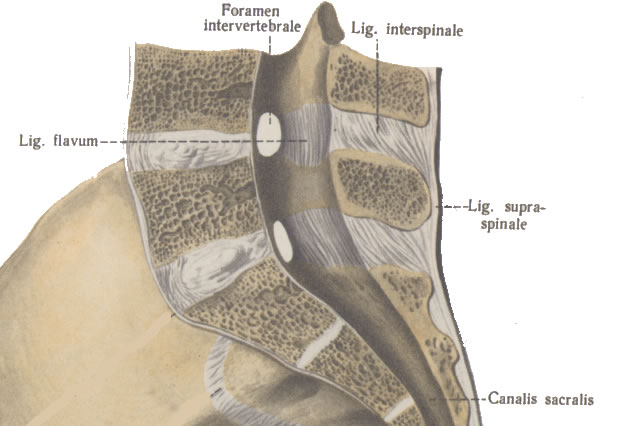
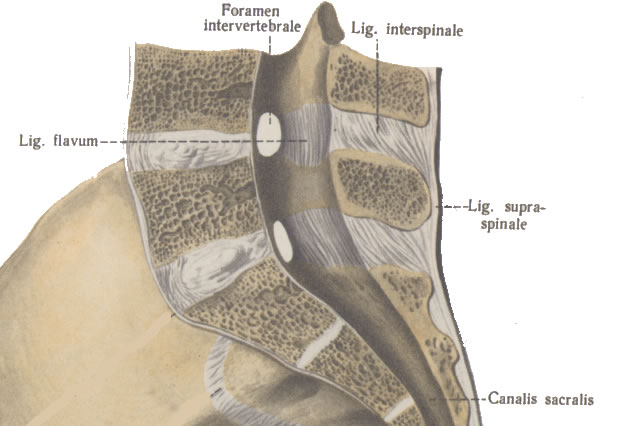
Fig-1: Normal anatomy of the lumbar spine:
midsagittal section.
The mean thickness of the end plate of the lumbar
disci was 1.03±0.24 mm for cranial (to disk) endplates and 0.78±0.16
mm for caudal endplates. For lumbar intervertebral disks, the
cranial endplate was significantly thicker and denser than the
caudal endplate (p<0.001-0.05). Thickness and BMD of endplates were
independent of age. Based on discography, a trend of more severe
disk degeneration associated with greater thickness in both the
cranial and caudal endplates was observed, and was most marked in
severely degenerated disks (p<0.05). However, no evidence was
detected for a link between more severe disk degeneration and
elevated endplate BMD (p>0.05).7
Biodynamic background:
The lordotic curve of the lumbar spine is around 50±10
degrees according to different factors. It is supposed to be equal
to the pelvic incidence which is fixed and equal to the sum of
sacral slope and pelvic tilt. These data are of concern when dealing
with multilevel fusion and presence of gross deformity of the spine
with discrepancies of the pelvic tilt exceeding more than 25
degrees.8 Considering these data the acquisition of
the intradiscal configuration is more logic than taking these data
to decide the degree of lordotic degree of the construct. Never the
less, the lumbar lordotic curve is more heavily dependant at the L4
to S1 levels, constituting 75% of the global value of the lumbar
lordosis. Patients
Imaging
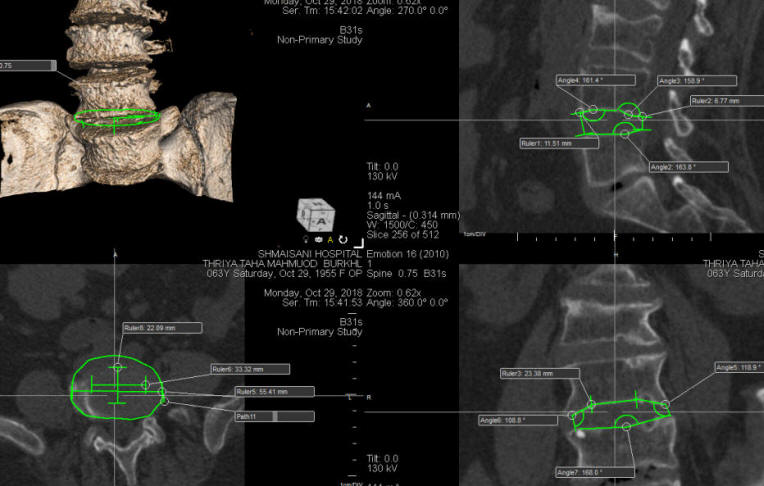
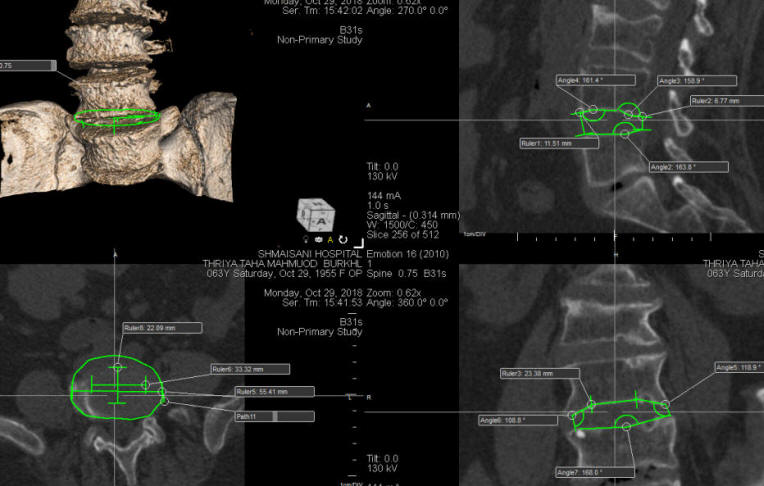
Fig-2: Measurements taken for L4-5 disc space in one patient.
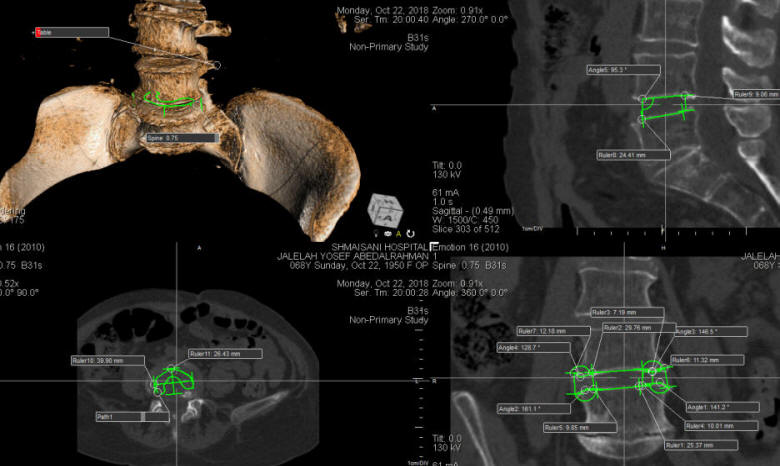
Fig-3: According to these data
obtained by ORS Visual software, the patient needs a cage total
width 30 mm, 10mm
height with 6 degrees lordosis.
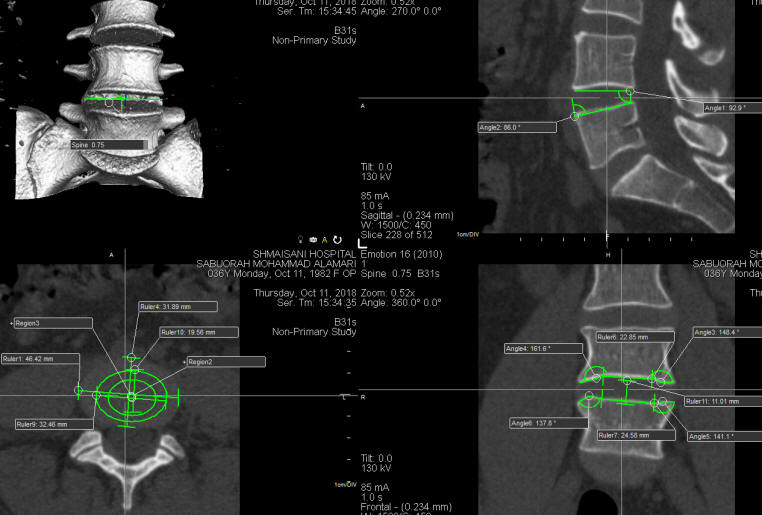
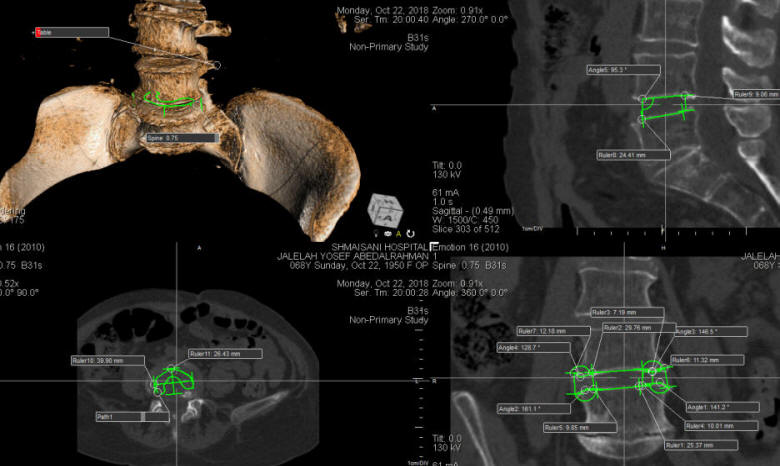
Fig-4: This case needs articulated cage 32 mm total
diameter, 11 mm height and 12 degrees lordosis according to the ORS
Visual data.
RESULTS
DISCUSSION
.
Advantages of this technology:
1. The recurrence rate will go down almost to zero, because the
device will aid support to the height of the disc space, preventing
the outer most part of the annulus fibrosis to slip to the vertebral
canal.
2. Restoring of the lordotic alignments and the height of the
collapsed disc space will augment the degree of postoperative
recovery. The LBP and radicular pain will be less than the standard
methods.
3. Working in fresh area is more easier than working in
postoperative recurrent disc with massive scars.
4. In certain cases the disc space height is different on both sides.
This technology will correct this problem.
5. There is no need to perform transpedicular screw fixation,
because the construct will yield this mission from within the disc
space with the use of the 2 lockers embedded in the articulated
cage. They have about 1.5 mm depth blade, sharp from all edges to
minimize surgical trauma to the endplates,
6. There will be no migration, nor loosening of the construct, since
it is placed at the anatomical groove in the disc space, avoiding by
this the escalation of avascular necrosis.
7. Posterior migration of the construct will be prevented by the
lordotic configuration of the construct. Anterior migration will be
prevented by the lockers and presence of some curve at the most
anterior part of the construct.
8. The MRI artifacts will be minimal, since the titanium lockers are
small and far from the dura.
9. In retrolisthesis, this technology can be used and can resolve
the retrolisthesis, by reducing the height of the disc space and
distracting the adjacent facets.
10. The harvested bone from the spinous process can be melted and
inserted at the site of the cavities, were the lockers situated,
avoiding during that the use of artificial bone graft and minimizing
the postoperative infection, inflammatory reaction or rejection.
11. The slim configuration of the construct with maximum width 7 mm
prevent dural force traction during insertion and keeping the
isthmus and facets intact with most stenotic anatomy of the area of
interest. The usual TLIF has a width of 10 mm.
12. The annulus fibrosis will be preserved, and can provide its
function at least partially. Limitations and disadvantages of
this technology:
1. This technology is not suitable for spondylolisthesis with gross
overmobility. In these
cases transpedicular screw fixation of the mobile segments is
mandatory.
Footnotes
Disclaimer: The author of this paper have received no outside
funding, and have nothing to disclose.
REFERENCES
1. https://www.neurosurgery.tv/recurrentprolapseddisc.html.
2. Posterior lumbar interbody fusion
with stand-alone Trabecular Metal cages for repeatedly recurrent
lumbar disc herniation and back pain. Michiel B. et al.
Neurosurgical Center Amsterdam, Neurosurgery Spine Clinic, Sint
Lucas Andreas Hospital, and Academic Medical Center, Amsterdam, The
Netherlands. J Neurosurg Spine 20:617–622, 2014 617 ©AANS, 2014
3. Complications of pedicle screws in lumbar and lumbosacral fusions
in 105 consecutive primary operations. P. C. Jutte R. M. Castelein ©
Springer-Verlag 2002. Eur Spine J (2002) 11 :594–598.
4. Painful Schmorl's node treated by lumbar interbody fusion. K
Hasegawa, A Ogose, T Morita & Y Hirata. Spinal Cord volume 42, pages
124–128 (2004)
5. https://www.neurosurgery.tv/pain/bprfinspinesurgery.html.
6. MECHANICAL DESIGN CRITERIA FOR INTERVERTEBRAL DISC TISSUE
ENGINEERING Nandan L. Nerurkar, Dawn M. Elliott, and Robert L. Mauck.
J Biomech. 2010 Apr 19; 43(6): 1017–1030. Published online 2010 Jan
18. doi: [10.1016/j.jbiomech.2009.12.001]
7. The osseous endplates in lumbar vertebrae: thickness, bone
mineral density and their associations with age and disk
degeneration. Wang Y1, Battié MC, Boyd SK, Videman T. Bone. 2011 Apr
1;48(4):804-9. doi: 10.1016/j.bone.2010.12.005. Epub 2010 Dec 17.
PublishMed.
8.Spinopelvic Parameters: Lumbar Lordosis, Pelvic Incidence, Pelvic
Tilt, and Sacral Slope. What Does a Spine Surgeon Need to Know to
Plan a Lumbar Deformity Correction? Paul C. Celestre, MD et al. |